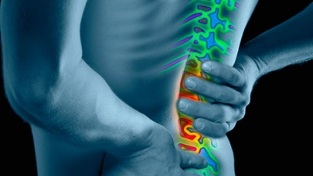
Although the idea is widespread, spinal osteochondrosis is not considered part of the aging process. The elastic discs between the vertebrae, like the shock absorbers, are responsible for bending and stretching the back. They wear out over time and no longer provide a full range of motion. With age, accidental injuries, including stress and minor injuries to the spine, can damage the back discs and cause osteochondrosis of the spine.
Who is affected by this back disease?

In most cases, the first symptoms of lumbar osteochondrosis occur between the ages of 11 and 12. The disease manifests itself openly by the age of sixteen, but the most severe course and most frequent complications occur between the ages of 15 and 20 years.
Children under the age of 15 rarely have severe forms of osteochondrosis, which are generally associated with an excellent condition of the musculoskeletal system, and especially the spine. In addition, the disease takes time to develop and takes an average of five years.
Fortunately, these diseases are easier to treat in children than in adults.
symptoms
Reflex syndromes
- Cervical- pain in the neck in different ways (pulling, tingling, shooting), a feeling of "crawling" in the cervical muscles, as well as a decrease in mobility and elasticity of the neck.
- Lumbagois a sharp, sharp pain in the lumbar region that can be accompanied by numbness or swelling. The words "lumbodynia" or "lumboischialgia" may be used instead of the word "lumbago. "
- Thoracic- Pain of a different nature that is always present in the chest, shoulder blades and ribs or occurs during physical activity.
Compression syndromes
Occurrence of pain syndrome in lumbar osteochondrosis is due to:
- Compression of root structures (radiculopathy).
- Spinal cord compression (myelopathy).
- Damage to the spinal cord due to impaired blood supply.
- Narrowing (stenosis) of arteries and veins (myelosuppression).
Diagnosis methods
Differential Diagnostics
Not every disorder can be diagnosed with a simple laboratory test. Many conditions cause similar symptoms. For example, many infections cause fever, headaches, and fatigue.
Causes many mental disorders:

- sadness;
- anxiety;
- sleep problems.
Differential diagnosis identifies possible disorders that cause symptoms. Typically, this diagnosis is based on several tests. These tests may exclude conditions and / or determine if you need additional testing.
Differential diagnosis is used to identify physical or mental health problems that cause similar symptoms.
Differential diagnosis is also often used in psychiatry / psychology, where a patient with symptoms of several diseases can be given two different diagnoses. For example, a patient diagnosed with bipolar disorder may be diagnosed with a borderline personality disorder based on the similarity of symptoms in both conditions.
Who is diagnosed more often?
Previously, the disease was diagnosed in sick people after 45 years, but today about 27% of adolescents suffer from some degree of osteochondrosis.
It is understandable that the disease is so widespread - children began to spend a lot of time in a sitting position due to computers and the Internet. Is this bad? Time will tell, but it remains true - the pay for a sedentary lifestyle is high, and osteochondrosis is far from the worst disease that can occur with such a lifestyle, but the most common (after obesity).
How to determine a disease and its degree?
first
Under normal circumstances, the intervertebral discs are constantly renewed, but the process slows down and a disease such as grade 1 osteochondrosis occurs.
There are many reasons for this:
- obez;
- metabolic diseases;
- immune deficiency, etc.
Unfortunately, the instability of pain in a certain degree of disease is due to the fact that many people neglect the diagnosis and treatment and try to treat the pain alone. To do this, use ointments and various tinctures. But this is the biggest mistake.
First-degree lumbar osteochondrosis can be easily treated by contacting a good specialist and performing a series of simple actions.
Grade 1 osteochondrosis is compression of the intervertebral cartilage in the lumbar region. The main symptom at this stage is a slight pain when turning or bending. Sometimes the symptoms are more severe and short-lived due to sudden movements or serious efforts.
seconds
An obvious sign of the disease is pain in the lower back, which increases with any movement. Pain can radiate from above the spine.
Pain with osteochondrosis can spread to the lower extremities.
The second stage of osteochondrosis is characterized by such severe pain that it manifests itself during coughing.
Additional symptoms are associated with pinched nerve endings:
- Sensitivity changes in the lower extremities. The main symptoms are: pain, numbness of the legs, high or very low sensitivity of the skin of the lower extremities.
- Limited mobility. A person suffering from osteochondrosis (grade 2) finds it very difficult to move as the disease progresses.
- Increased fatigue and persistent sleep. The patient has chronic fatigue accompanied by irritation. This symptom is explained by the pain syndrome that constantly worries a person.
- Problematic urination and pain in the kidneys.
Third

When the patient reached Stage 3, his posture changed significantly. In more advanced cases, bone deformity occurs. At this stage of lumbar osteochondrosis, the patient's general physical and / or mental condition is clearly deteriorating and there is a deep loss of energy.
The third stage is characterized by the appearance of narrowing of the intervertebral foramen against the background of previous changes. Intervertebral disc herniation occurs, blood vessels in the neck and muscles are damaged. The patient has dizziness, pain in the back of the head.
Fourth
The terminal phase occurs when the intervertebral disc is degenerated and the disc space is destroyed. At this stage, the disc thinning reaches a maximum or, worse, disappears completely. Postural imbalance is acute and movement and elasticity are extremely limited.
Stage 4 lumbar osteochondrosis is often characterized by severe pain and higher physical and / or mental deterioration. There is a permanent loss in both growth and energy levels. Stage 4 is generally considered irreversible.
doctor's advice
Which doctor should I contact?
When independent treatments stop having analgesic effects, the patient begins to ask himself: which doctor treats osteochondrosis? The first person you can contact to treat lumbar osteochondrosis is your local therapist. But in this case, he plays the role of a dispatcher, because he will not be able to prescribe a complete treatment - this is not his specialty.
Most likely, he will send you to a neurologist. It is this specialist who will conduct the necessary research and help you develop a treatment program. The therapist may also refer you to a vertebrologist. This doctor deals directly with spinal diseases.
Scales and tests
Quality of life assessment

A generalized feature, such as quality of life, is especially important for a group of patients with a disease because they can affect the effectiveness of treatment. This is especially important for comparing the results of several studies, economic analysis, and understanding the problem as a whole.
Methods of assessing quality of life include:
- Oswestry quality of life survey.
- Roland-Morris questionnaire.
- Stratford Scale.
- Quebec Back Pain Scale - a survey on how back pain affects your daily life).
Pain Scales
Pain is an unpleasant feeling and emotional experience associated with tissue damage. The goal is to keep the body responding and prevent further tissue damage.
Methods for assessing pain syndrome include:
- Corf won the Chronic Pain Assessment Scale.
- McGill Pain Questionnaire.
- Oral Pain Scale.
Evaluation of treatment outcome
- McNab's Subjective Rating Size.
- Patient satisfaction scales.
- Prolo functional and economic result scale.
- Lumbosacral Outcome Scale.
- Nurik Size.
Hardware test
x-ray
X-rays provide detailed bone structures of the spine and are used to exclude the resulting back pain:
- Spondylolisthesis.
- Tumors.
- Cracks.
Calcium in bone prevents X-ray penetration, and the appearance of bones is perceived as a shadow in the film. Because bone is mainly composed of calcium, X-rays provide a perfect view of all details. However, discs and nerve roots do not contain calcium, so X-rays do not capture images of these structures. Therefore, X-rays cannot be used to diagnose a herniated disc or other causes of a compressed nerve.
X-rays should not be taken in pregnant women.
Complications and possible consequences
Complications and possible consequences of lumbar osteochondrosis include:
- Radiculopathy is a disease characterized by nerve root disease.
- Muscle Weakness - Common symptoms include fever, fatigue, flu-like symptoms, paresthesias, weight loss, and changes in consciousness.
- Neurogenic bladder - a nerve problem that controls the bladder and urination
- Damage to lower motor neurons.
- Raynaud's phenomenon is the narrowing of the capillaries of the fingers and toes, where spasms occur.
- Pain in the neck, back, legs.
Treatment
Treatment may vary depending on the severity of your symptoms and how much you limit your daily activities.
Here are some treatments that your doctor may prescribe based on your pain level:
- Non-surgical treatment- not all patients with osteochondrosis require surgery. More conservative treatments for mild to moderate pain.
- Spondylodesis- surgery in the treatment of osteochondrosis.
Prevention

Prevention of osteochondrosis of the lumbar segment is to eliminate the risk factors that cause this disease. Elimination of factors is the main preventive measure.
Physical activity is normalized, lumbar muscles are strengthened, the maximum load on the lumbar spine is prevented, the development of diseases that cause back pain is prevented, all of which are prophylactic to prevent the symptoms of lumbar osteochondrosis.
Moderate exercise, lifestyle changes, and good nutrition can help prevent painful and disabled symptoms.
If you see signs of lumbar osteochondrosis, do not squeeze and see a doctor immediately. A disease that is detected in time is easier to treat and continues to be ineffective.























